Plantar Fasciitis
The plantar fascia is a band of tissue, similar to a tendon, which runs from the front of the heel bone (calcaneus) to the ball of the foot (metatarsals). This dense strip of tissue helps to support the arch of the foot and acts as a rubber band to absorb shock as you walk.
When the foot is on the ground the full weight of the body is concentrated on the plantar fascia. This force stretches the tissue as the arch of the foot tries to flatten from the weight of the body. This leads to stress on the plantar fascia where it attaches to the heel bone. Small tears of the fascia can happen. However, the body normally repairs these tears.
As this process of injury and repair repeats itself over and over again, inflammation of the plantar fascia occurs resulting in plantar fasciitis/fasciosis. Commonly associated symptoms may include pain when getting out of be in the morning or after sitting, recurrence of pain throughout the day, heel pain after long periods of standing and pain that increase over a period of months.
An accurate clinical examination by a podiatrist is required to ensure the most suitable treatment is undertaken. Diagnostic imaging such as X-rays and Ultrasounds may be ordered to further assist the examination.
Treatment
The treatment of plantar fasciitis may involve rest, ice and Nonsteroidal anti-inflammatory medication (NSAIDs) which will help with pain and swelling. Physical therapy such as stretching, taping, dry needling and supportive footwear may be performed to help stabilize the foot and ankle. Orthotic therapy may be used involving a custom made orthotic device placed inside the shoe that can help address any biomechanical factors to reduce the stress on the plantar fascia.
Most people will respond to these conservative measures, however some may require an injection in the heel (Prolotherapy or corticosteroid) to help with the pain, or in the worst cases may require surgery to treat chronic cases.
Achilles Tendon Pain/Tendonitis
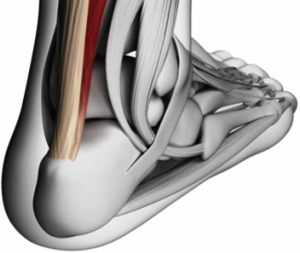
 The Achilles tendon is the largest and strongest tendon in the body. It connects the 2 large calf muscles (the gastrocnemius and soleus) to the back of the heel bone (calcaneus). The tendon gives us the ability to rise up onto our toes and is very important in facilitating walking and running. Forces up to 12 times body weight may arise during sporting activities.
The Achilles tendon is the largest and strongest tendon in the body. It connects the 2 large calf muscles (the gastrocnemius and soleus) to the back of the heel bone (calcaneus). The tendon gives us the ability to rise up onto our toes and is very important in facilitating walking and running. Forces up to 12 times body weight may arise during sporting activities.
Achilles pain is usually a result of tendinitis caused by tight or fatigued calf muscles which transfer too much of the burden of walking or running to the Achilles tendon. The tendon becomes inflamed and over time can produce a covering of scar tissue which is less flexible than the tendon. Achilles tendinopathy can vary in severity from a mild pain during an activity to more severe cases of tears or even rupture.
Symptoms usually include pain that can be a dull or sharp anywhere along the back of the tendon worse after rest or excessive activity. A nodule of scar tissue can often be felt on the tendon and local swelling and redness can occur about 2-3cm above the heel bone. Often there is also limited ankle flexibility and onset of pain when increasing mileage whilst running.
Achilles tendonitis is most commonly related to overuse and continues stress of the tendon. Not stretching the calves properly, excessive hill running, sand running or speed work, all of which stress the Achilles more than other types of running, can bring on Achilles tendinitis. People who over-pronate (their feet roll too far inward on impact) are most susceptible to Achilles tendinitis.
Treatment
To help prevent Achilles tendinitis stretching the calf muscles is important. Wearing the right shoes, strapping, strengthening exercises and orthotic therapy to address any biomechanical abnormality is important to help normalise the pressure and strain on the tendon. Therapies that can be performed at home including rest, ice and nonsteroidal anti-inflammatories are important until the Achilles is pain free and then ease back into any running or walking program.
For some cases where the Achilles pathology does not improve, injection therapy (Prolotherapy) may be required.
REMEMBER ACHILLES TENDINITIS CAN LEAD TO TEAR AND RUPTURE. IF IN DOUBT REST AND GET A MEDICAL PROFESSIONAL OPINION
Sever’s disease (Calcaneal Apophysitis)
Sever’s disease (calcaneal apophysitis) is the most common cause of heel pain in children. Sever’s disease is a painful inflammation in the growth plate area at the back of the calcaneus (heel bone) where the Achilles tendon attaches. It is most common in physically active children between the ages of 8 and 14 years old. Children most commonly report pain during periods of rapid growth and commonly gets misdiagnosed as ‘growing pains’.
Pain is usually felt at the back of the heel and Achilles tendon. There is often swelling on the heel, stiffness of the calf muscle in the morning and tender to touch. Additional symptoms reported by children also include;
- heel pain during physical activity increasing after exercise
- running and jumping make the symptoms worse
- in severe case children may limp and even have a tendency to tiptoe
- squeezing the sides of the heel bone is often painful
Sever’s disease is primarily caused by overuse or repeated minor trauma to the heel. Tight calf muscles are a common cause in children who develop this problem. There is a strong pull from the Achilles tendon (calf muscle) causing an pain, inflammation and irritation at its attachment on the growth plate at the back of the heel.
Some risk factors associated with Sever’s disease include;
- sporting activities that involve running and jumping more common on hard surfaces (basketball, soccer, football, netball)
- sporting activities that involve fast explosive movements (sprinting, athletics)
- a flat foot (over pronated) creates a twisting of the Achilles tendon adding to the shear forces of the tendon pulling on the heel bone
- adolescent obesity
- exercising while wearing inappropriate shoes
Treatment
A comprehensive podiatric assessment is recommended early to prevent the progression of symptoms and ensure appropriate treatment is undertaken. Diagnostic imaging including a X-ray and Ultrasound may be required for further diagnosis. At Sydney Foot Clinic the treatment options offered for children with Sever’s include;
- Rest – cutting back on sporting activity is essential to improve symptoms. If symptoms continue to be displayed then a complete break from sport may be needed
- ice and elevation
- an exercise program to stretch the calf muscle reducing pain in the symptomatic area
- massaging of the calf muscles
- heel raises or possibly a custom orthotic insole may be needed to reduce the sheer process exerted by the Achilles tendon on the growth plate/heel bone.
- strapping or taping of the ankle/foot
- avoid barefoot walking/running
- advice on appropriate footwear – running shoes, football/soccer boots
Heel spur syndrome
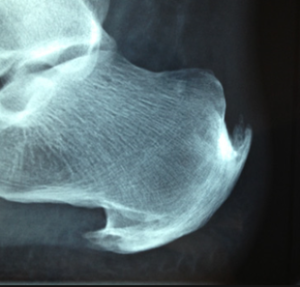
Heel spurs are abnormal growths that develop at the back or under the heel causing inflammation and pain.
Heel spurs develop and sometimes associated with plantar fasciitis and usually chronic plantar fasciosis. It is important to be aware that heels spurs may or may not cause symptoms in patients Pain may be worse when standing for long periods of time, worse in the morning or during particular physical activities such as walking and running.
Treatment
Digital imaging particularly X-rays may be prescribed by the podiatrist for further diagnosis of the heel spur. In many cases non-surgical treatment commonly relieves pain. At Sydney Foot Clinic the treatment options offered include;
- rest, ice, nonsteroidal anti-inflammatory medications and compression bandage to help relieve symptoms
- footwear advice and cushioning
- a custom made insole that provides cushioning and support
- dry needling
- prolotherapy injection therapy
Sometimes surgery may be required particularly for those patients with chronic heel pain. Surgery may involve release of the plantar fascia or removing the bony heel spur.