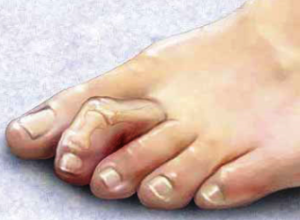
Hallux Abducto Valgus (Bunion)
A bunion is often described as a bump on the side of the big toe. But a bunion is more than that. The big toe leans toward the second toe, rather than pointing straight ahead. This throws the bones out of alignment – producing the bunion’s “bump.”
Bunions are progressive, they don’t go away, and will usually get worse over time. But not all cases are alike – some bunions progress more rapidly than others. As the bunion progresses, the big toe joint fails to function properly leading to arthritis in the joint. Osteoarthritis can develop in the big toe joint as the bunion worsens over time, causing increased pain and stiffness in the joint.
Causes
Bunions are most often caused by an inherited faulty mechanical structure of the foot. It is not the bunion itself that is inherited, but certain foot types that make a person prone to developing a bunion. Although wearing shoes that crowd the toes won’t actually cause bunions, it sometimes makes the deformity get progressively worse. Some other common causes include;
- footwear – high heels and tight fitting footwear
- poor foot mechanics
- trauma
Symptoms
Symptoms that may appear as a result of the bunion include;
- bump of the side of the big toe joint
- Pain and soreness
- Inflammation and redness.
- Burning sensation and possible numbness
- Corns or callus (hard skin) on the bottom or side of the big toe joint
- Stiffness moving the joint
Diagnosis
Bunions are most readily apparent – the prominence is visible at the base of the big toe or side of the foot. However, to fully evaluate the condition, the podiatrist at Sydney Foot Clinic may take x-rays to determine the degree of the deformity and assess the changes that have occurred.
A comprehensive assessment and biomechanical assessment may also be performed to identify any biomechanical
Treatment
At Sydney Foot Clinic, the following treatment options are offered for bunions;
- Nonsteroidal anti-inflammatory medications (NSAIDs) and Ice- help reduce the pain and inflammation.
- Padding and strapping the foot.
- Prescription of custom made orthotics – orthotics are designed to guide the posture/mechanics of the foot and reduce pressure at the big toe joint
- Footwear recommendations – advice regarding comfortable and supportive shoes.
- Injection therapy – prolotherapy can be used to reduce symptoms.
- Activity modifications.
- Splinting the big toe joint.
Because bunions are progressive and there is no effective treatment to get rid of them, surgery is sometimes indicated.
Hammer toes/Claw toes
Hammer toe, claw toes and mallet toes are common occurring lesser toe deformities. A hammertoe is a bending of one or both joints of the second, third, fourth, or fifth (little) toes. This abnormal bending can put pressure on the toe when wearing shoes, causing problems to develop.
Hammertoes usually start out as mild deformities and get progressively worse over time. In the earlier stages, hammertoes are flexible and the symptoms can often be managed with non-surgical measures. But if left untreated, hammertoes can become more rigid, cross over other toes reducing the affect of conservative treatment.
Symptoms
The bending of the toes can cause your toes to dig into the soles of your shoes forming painful calluses and corns either on the toe or the balls of the feet. Some other symptoms include;
- Pain or irritation of the shoe when wearing shoes
- Corns and calluses
- Inflammation or a burning sensation
- Possible numbness
- Footwear difficulties
- Upwards bending of toes – toes overlapping each other
Cause
The most common cause of hammertoe is due to an imbalance between a muscle/tendon. This imbalance can be as a result of particular foot types (flat feet and high arch feet) leading to a bending of the toe/s as a result from mechanical (structural) changes in the foot that occur over time in some people. Hammertoes may be aggravated by shoes that don’t fit properly. A hammertoe may result if a toe is too long and is forced into a cramped position when a tight shoe is worn. Some other causes of hammer toes are;
- Bunions – pressure from a bunion pushing onto the second toe causing a hammer toe and occasionally the second toe rising and overlapping the bunion
- Trauma
- Hereditary/genetics
Treatment
Preventing hammer toes from occurring is most affective treatment for lesser toe deformities. Such preventative measures include;
- Avoid wearing tight or narrow shoes (make sure shoes are not short – thumb space from your longest toe – not always your big toe!)
- Avoid high heel shoes
- If you have a wide foot wear wide fitting shoes
Conservative treatment offered at Sydney Foot Clinic for lesser toe deformities (hammer/claw/mallet) include;
- Removing calluses and corns – a podiatrist is trained to remove calluses and corns in a safe manner.
- Prescription of custom made orthotics – orthotics are designed to guide the posture/mechanics of the foot, reduce pressure at the lesser toe deformities and help control muscle/tendon imbalance.
- Splinting – some hammer toes can be splinted to help reduce the deformities
- Padding the foot – padding can redistribute pressure from the ball of your foot
- Footwear recommendations
- If conservative treatment fails, surgery may be needed to reduce rigid and symptomatic hammer toes.
Morton’s Neuroma (Intermetatarsal Neuroma)
A neuroma is a thickening of nerve tissue (Perineural Fibrosis) that may develop in various parts of the body. Morton’s Neuroma are a painful condition where a benign enlargement of nerve tissue forms between the third and fourth metatarsals/toes. This thickening of the tissue around the nerve causes foot pain, odd sensations, or numbness over the ball of the foot.
The thickening, or enlargement is the result of compression and irritation of the nerve. This compression creates enlargement of the nerve, eventually leading to permanent nerve damage.
Causes
Irritation or compression of the nerve between the ends of the metatarsals can lead to the development of a Morton’s Neuroma. Some other contributing factors in the development of a Morton’s Neuroma include;
- Trauma – injury to the area that may cause inflammation, swelling or nerve damage may lead to a Neuroma.
- Footwear – wearing shoes that cause toes to be squeezed together causing swelling and inflammation leading to a neuroma (narrow shoes, tight shoes, poorly fitting shoes).
- Foot type – flat feet (pronation) or high arch (supinated) feet can increase changes or irritation/compression of the nerve between the metatarsals leading to a Morton’s Neuroma.
- Physical activity – repetitive stress at the all of the foot during activities such a running can cause irritation of the nerve.
Symptoms
Most commonly patients suffering from a Morton’s Neuroma will feel pain at the space between their 3rd and 4th toes. Other symptoms often reported by patients include;
- Tinging, burning or numbness of your toes and the ball of your foot
- Pain between the toes and the forefoot
- A feeling as if you are standing on a pebble in your shoe
- Increase in pain with activity or tight fitting shoes (high heels, narrow shoes)
Treatment
A comprehensive podiatric assessment is recommended to prevent the progression of symptoms and ensure appropriate treatment is undertaken. Diagnostic imaging including a X-ray, Ultrasound and often a MRI may be required for further diagnosis. At Sydney Foot Clinic the following treatments are offered to treat Morton’s Neuroma;
- Padding/offloading – offloading excess pressure from the ball of the foot.
- Custom Orthotic therapy – prescription of a custom orthotic placed in your shoe will address any biomechanical factors and reduce irritation/compression of the nerve.
- Footwear recommendations – avoiding high heels (increase pressure on your forefoot), narrow or tight fitting shoes will reduce the symptoms of the neuroma.
- Injection therapy – specialized injections can be used to infiltrate the area surrounding the nerve to reduce inflammation and reduce compression.
- Education regarding activity changes.
- Nonsteroidal anti-inflammatory medications (NSAIDs) and Ice- help reduce the pain and inflammation.
If conservative treatment does not relieve symptoms surgery may be necessary to reduce the symptoms.
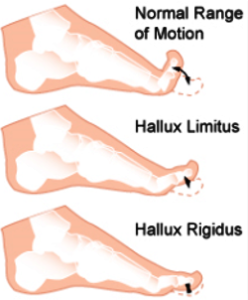
Hallux Limitus/Rigidus (Big toe stiffness)
Hallux rigidus is a disorder of the joint located at the base of the big toe. It causes pain and stiffness in the joint, and with time it gets increasingly harder to bend the toe.
In its earlier stage, when motion of the big toe is only somewhat limited, the condition is called “hallux limitus.” But as the problem advances, the toe’s range of motion gradually decreases until it potentially reaches the end stage of “rigidus,” in which the big toe becomes stiff, or what is sometimes called a “frozen joint.” ‘Hallux” refers to the big toe, while “rigidus” indicates that the toe is rigid and cannot move. Hallux rigidus is actually a form of degenerative arthritis.
This disorder can be very troubling and even disabling, since we use the big toe whenever we walk, stoop down, climb up, or even stand. Many patients confuse hallux rigidus with a bunion, which affects the same joint, but they are very different conditions requiring different treatment.
Causes
In some people, hallux rigidus runs in the family and is a result of inheriting a foot type that is prone to developing this condition. In other cases, it is associated with overuse and trauma. Some other causes of hallux limitus include;
- Foot type – excessive flat feet (pronation) or high arch feet (supinated)
- Trauma – stubbing your toe
- Inflammatory diseases – gout or rheumatoid arthritis
- Repetitive stress on the big toe joint – activities that require a lot of squatting
- Length of first metatarsal bone – excessively long or short metatarsal
Symptoms
Early signs and symptoms of hallux limitus include;
- Pain and stiffness in the big toe during use (walking, standing, bending).
- Callus formation underneath or the side of the big toe.
- Difficulty performing certain activities (running, squatting).
- Swelling and inflammation around the joint.
- Difficulty wearing shoes.
- Dull pain in the knee, hip or lower back due to a change in gait (way you walk).
Treatment
The sooner this condition is diagnosed, the easier it is to treat with conservative methods. Therefore, the best time to see a podiatrist is when you first notice symptoms. If you wait until bone spurs develop, your condition is likely to be more difficult to manage.
At Sydney Foot Clinic, the podiatrist in diagnosing hallux rigidus will examine your feet and move the toe to determine its range of motion. Medical imaging such as X-rays will most often be prescribed help determine how much arthritis is present as well as to evaluate any bone spurs or other abnormalities that may have formed.
At Sydney Foot Clinic the following treatments are offered to treat Hallux Limitus;
- Shoe modifications – Shoes with a large toe box put less pressure on your toe. Stiff or rocker-bottom soles may also be recommended.
- Custom Orthotic therapy – prescription of a custom orthotic placed in your shoe will address any biomechanical factors (flat feet or high arch feet) reducing the stress and pressure at the big toe joint. Orthotics can also be used to splint/brace the big toe if Hallux Rigidus is present.
- Injection therapy – Prolotherapy can help reduce symptoms and offer relief.
- Medications – non sterioidal anti-inflammatory medications (NSAIDs) and Ice- help reduce the pain and inflammation.
In some instances and progressed deformities conservative treatment may fail and surgery may be required to reduce pain and relieve symptoms.
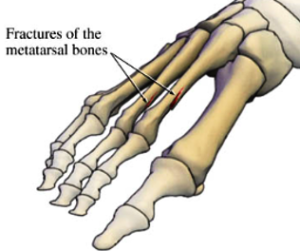
Stress Fracture
Stress fractures are tiny, hairline breaks that can occur in the bones of the foot. They can be caused by overtraining or overuse, improper training habits or surfaces, improper shoes, flatfoot or other foot deformities, and even osteoporosis. These tiny breaks in the bones of the feet can lead to a complete break if left untreated.
Causes
Some common causative factors of stress factors are;
- Running on hard, uneven surfaces.
- Trauma
- Inappropriate footwear – poor support or poor cushioning
- Biomechanical factors – overpronation (flat feet) or supination (high arch feet) resulting in increased force at particular aspects of the foot
- Osteoporosis – weakening of bones leading to stress fractures
- Exercise program – intensity, frequency and duration of training
Symptoms
Stress fractures commonly occur in the metatarsal bones of the feet, the tibia (shin bone), navicular and femur (thigh bone). Some symptoms of a stress fracture may include pain and swelling, particularly with weight bearing on the injured bone. Some other symptoms associated with stress fractures include;
- Pain, swelling and warmth at the site of injury
- Redness and bruising at the injured site
- Pain increased with activity
- Difficulty putting shoes on
- Throbbing
Treatment
A comprehensive podiatric assessment is recommended to prevent the progression of symptoms and ensure appropriate treatment is undertaken. Diagnostic imaging including a X-ray is used to diagnose a stress fracture. In some cases the fracture may not show up on the X-ray until a couple weeks after the pain starts. Patients are advised to temporarily stop activities that cause the stress fracture during the six to eight weeks it may take for the fracture to heal.
At Sydney Foot Clinic we will attempt to immobilise the bone for a period of six to eight weeks which is usually sufficient. Upon this rehabilitation is performed to ensure you are able to return to normal activities. Some other treatment options available for stress fractures include;
- RICE protocol – rest, ice, compression and elevation will help relieve symptoms
- Adequate footwear – cushioning and supportive helping to redistribute forces throughout the rest of the foot
- Modification of training program – changing intensity, duration, frequency and surface trained on.
- Immbolisation